无论你刚刚被诊断或担心,你可以有乳癌,你可能紧张,困惑,绝对惊。这是正常的,每个人都特色在HealthCentral与大病感觉就像你现在要做的。但是,我们和他们,在这里为您服务。On this page alone, you’ll discover not only the realities and challenges of the condition, but also the best treatments, helpful lifestyle changes, wisdom from people who have been where you are now, and all the critical information you need to help you not just manage—but thrive. We’re sure you’ve got a lot of questions...and we’re here to answer them.
我们的专业面板乳腺癌
我们去了一些国家的顶尖专家,在乳腺癌给你带来最先进的最新信息成为可能。

P. Hank Schmidt, M.D.Breast Surgical Oncologist

乔纳森Stegall,医学博士医疗主任

扎西米特里,医学博士乳腺癌肿瘤科
What Is Breast Cancer, Exactly?
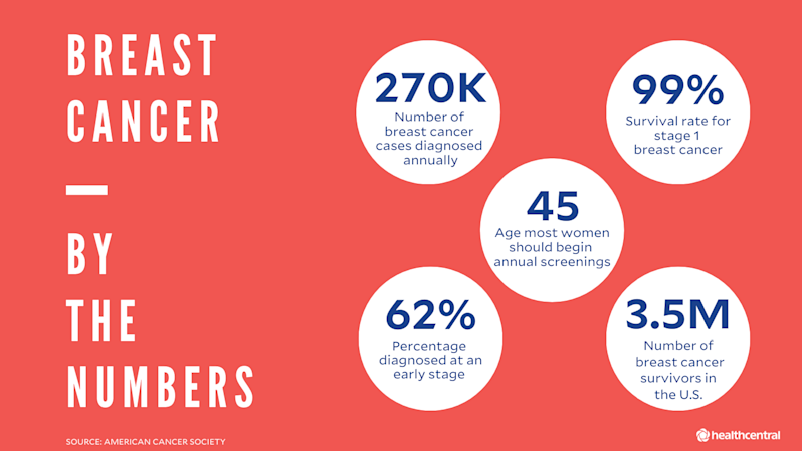
If you have boobs or know someone who does, you likely know some of the breast-cancer basics because there’s a darn good chance there’s a person in your life who’s had it. Breast cancer is the most common malignancy in women—about 270,000 cases are diagnosed each year—accounting for approximately 30% of all cancer cases, according to the American Cancer Society. Although it happens much less often, men can also develop breast cancer. In fact, Beyonce’s dad recently became one of the 2,670 men diagnosed annually.
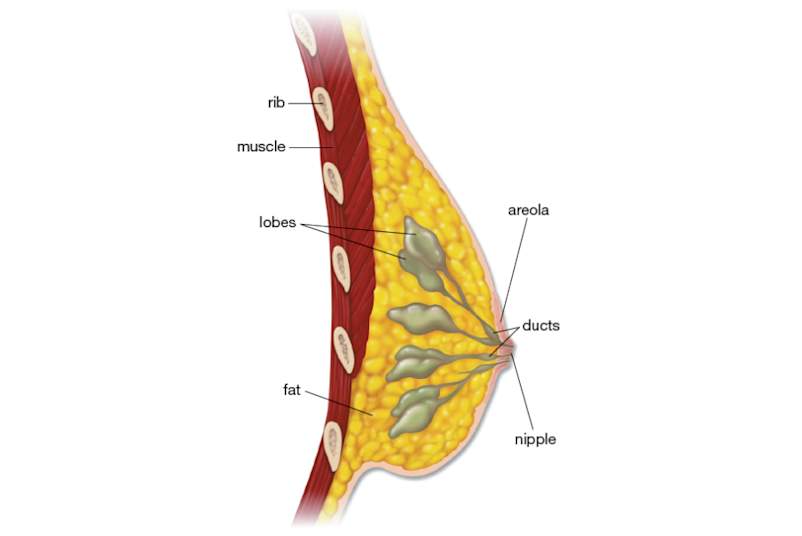
In each of these people, their breast cancer began the same way: A rogue cell began to multiply in ways it’s not supposed to, eventually forming a tumor. To really understand the different types and stages of breast cancer, it helps to have an image in your mind of where it starts and how it grows. The main structures of the breast are milk glands (called lobules), the ducts that carry milk, and fatty and fibrous tissue that make up most of the breast. Most breast cancers start in the glands or ducts.
Once breast cancer is found, doctors will give it a stage—from 0 to IV—depending on the extent of the disease, what the prognosis is, and which treatments will work best. Within each stage, there are further classifications depending on things like tumor size and lymph-node involvement, usually indicated by doctors with the letters a, b, and c. For now, we’re sticking with the main categories:
0级:原位也称为导管癌(DCIS),0期肿瘤是异常细胞,其形式在管道内(“原位”剩余到位装置),和目前的研究表明,在很多情况下,这些细胞不会生长的任何进一步或原因问题的病人。有人甚至认为DCIS癌前病变的这种非侵入性的形式。
收获?约20%至的30%的时间,将这些细胞继续外的控制他们的方式和推入组织中的导管以外(这被称为“侵入性”癌症)。不幸的是,没有肯定的方式来知道你有哪种类型的DCIS的,这就是为什么即使0期乳腺癌的治疗(详见下文)。
Stage I:这是浸润性乳腺癌的尽可能早的阶段。在这一点上,肿瘤为不大于20毫米(2cm)上,并与没有扩散超过微观到腋下淋巴结。在这个阶段,抓住癌症是可以治愈和治疗:五年生存率,意义,妇女谁是活着五年后诊断,是一个令人难以置信的99%的数量。
Stage II:这些肿瘤确实试图赌注他们的要求。他们一般大于20毫米以上,并可能蔓延到手臂几下淋巴结。但是深呼吸。II期癌症的五年存活率是一个仍然是一个令人放心的85%。
Stage III:在这一点上,所述肿瘤是可能相当大(大于50mm)的和/或癌细胞已经作出自己的方式分为以下几种淋巴结,或者下臂或远在锁骨。这个阶段还包括在直接侵入胸壁或已经形成皮肤结节或溃疡癌症。
Stage IV:This most advanced form of breast cancer, known as metastatic, has spread to the bones and/or organs, such as lungs, liver, or brain. The most difficult part about this diagnosis is that it’s not considered curable. However, in some people, progression of the disease can be slowed or even stopped by a series of medications and other treatment, and the disease becomes more of a chronic illness. The five-year for this stage is 27%, which we know isn’t easy to see, but here’s what you must remember about these stats: Yes, they are scary, but你是不是一个数字。有女今天还活着谁一直患有转移性乳腺癌的几十年。
不太常见的癌症和其他乳腺疾病
值得注意的是:以上介绍最常见的乳腺癌,但也有few less-common types你应该知道,而且有时与乳腺癌混淆其他一些乳腺疾病。
- Paget病:This rare breast cancer starts in the milk ducts and then spreads to the skin of the nipple and areola. It can look like an eczema rash.
- 炎性乳腺癌:In these cases, the cancer is typically more advanced, according to the National Cancer Institute, and has spread to the skin of the breast, making it red, swollen, and sometimes dimpled like the skin of an orange. With IBC, you may not always feel a lump, and it tends to be more common in younger women and those who are African-American.
- 小叶原位癌:尽管在名称中的“癌”,原位(LCIS)小叶癌是不是癌症。在集装箱检查系统,细胞就在乳房的腺体奶异常生长,但他们不侵入其它组织。虽然这个条件isn’t癌症,这是一个标志,一个人是在为在未来无论是乳腺癌患癌症的风险增加,而你很可能需要更频繁的场次。

生活转移性乳腺癌
Dionna科瓦尔分享她的转移性乳腺癌和寻找治愈的故事。点击了解更多。
What Causes Breast Cancer in the First Place?
Exactly what triggers breast cells to grow out of control isn’t well understood, but scientists do know that certain factors and habits can interfere with a cell’s instruction manual, aka its genes, according to the American Cancer Society. If something blocks its signal to stop dividing or messes with its ability to repair DNA damage, those abnormal cells will just keep on going.
每个人的风险是不同的,取决于多种因素,如遗传,家族史,生活方式等问题。但女性平均拥有约在她的生活中患乳腺癌的12%的机会。The average age of diagnosis is 62.
这里有一些乳腺癌最常见的危险因素:
Family history:有一个近亲(母亲,父亲,姐妹),或谁已经有疾病可以使你的风险更高一些更遥远的亲戚。妇女与BRCA1或2突变在其一生中患乳腺癌的50%至85%的风险。通常情况下,这些基因有助于防止异常生长;但是当他们损坏,它很难为人体短路肿瘤的发展。
不是每个人都需要对这些突变进行测试,但那些与某些类型的家族病史的(例如,具有与乳腺癌两个第一亲属或一个,如果你有德系犹太人的遗产)应该。所以,在您下次的检查,询问你的医生,如果你要考虑基因筛查,以得到你患乳腺癌几率更好的手感。如果事实证明你确实有突变的一个,你就可以将工作与你的医生在一个计划,让那些风险数量下降。
年龄:只是年纪越来越大的增加患乳腺癌的风险,而这种疾病大多数情况下的人中,50岁以上的发生。有时需要几十年的小基因突变积累的一个终于打破这种平衡之前并触发肿瘤。
Hormones:大多数乳腺癌是由雌激素和孕激素刺激,所以不再是一个女人暴露生殖激素,乳腺癌的高她的风险。谁12岁以前开始时期女性对患乳腺癌比别人更高20%的几率约30%后,55岁增加14岁命中绝经后谁开始的赔率与通过变化去10年前。以结合雌激素和孕激素治疗更年期症状也增加风险(多少要看你怎么老是你多久采取了药物治疗)。使用某些口服避孕药避孕的历史也与风险非常小(7%)的增加。
体内脂肪:下面是关于有点肥知的事实:它产生雌激素。所以,你有更多的,较高的激素水平往往是。在一项研究中JAMA Oncologyfound that in post-menopausal women, the risk of an estrogen-sensitive tumor was about twice as high in those with the highest percentage of body fat compared to the lowest. This was true even for women who had a “healthy” body-mass index.
醇:Look, you can still enjoy a cocktail now and then, but even moderate drinking (one to two drinks a day) may increase the risk of breast cancer by about a third to a half, according to a study in目前乳腺癌报告。
家庭计划:无论你有孩子或不和在什么年龄可以通过改变你的程度,暴露于激素影响你患乳腺癌的风险。在研究国际癌症杂志发现谁从未有过的孩子们分别为1.3倍更容易患上这种疾病的妇女...妇女谁了他们的第一个孩子后,35岁分别为1.4倍更有可能得到乳癌谁比那些岁之前有一个孩子20.尽量不要到太挂在这些数字虽然:有没有人建议青少年怀孕预防乳腺癌?不。有一个孩子的正确时间,只要你说的是,这可能是永远。
Do I Have the Symptoms of Breast Cancer?
Some breast cancers cause no obvious symptoms在所有这就是为什么定期乳腺X线检查是非常重要的。(美国癌症协会说,女性需要每年乳房X线照片开始在45岁,但应该有开始在40年筛选选项)虽然有时,这些肿瘤也让自己知道你,所以它有助于有什么样子的感觉对于。有以下任何症状并不一定意味着你有癌症。相反,考虑他们的信号打电话给你的医生:
肿块和肿胀:很多女性有自然乳房结块。You should take note of any lumps you feel or see in your breasts—but if both boobs have similar lumps in similar places, or they come and go with your menstrual cycle and are smooth and rubbery, they’re likely just cysts or other normal clumps of tissue. The lump to pay most attention to is one that’s new, only on one side, and doesn’t go away.
另一件事要知道:虽然肿瘤可以感受到湿软和光滑的触感,癌肿块往往具有不规则边缘和手感较硬和不动产,像鹅卵石。部分或全部一个乳房的肿胀无法解释也应检查出来。已经扩散到淋巴结有时更先进的乳腺癌患者也可引起肿胀,压痛,或在腋下或锁骨的质量。
痛:许多妇女体验乳房胀痛很快就会和在月经周期的某段时间去,但新的疼痛,不走你的期间应签出。
乳头的改变:一个新缩回(或在凹陷)乳头是在一些癌症的症状。甲肿瘤可以在拖船该组织向内引起炎症和疤痕。这同样适用于突发性乳头溢液,尤其是流体这就是血性,在人谁不哺乳或曾在去年一个孩子。和周围的乳头湿疹样皮疹可能是Paget病的征兆。
皮肤的变化:Redness, warmth, swelling, or dimpling could point to inflammatory breast cancer.
We've got all the details on breast cancer signs and symptoms. Click here to learn about it all.
Read MoreHow Do Doctors Diagnose Breast Cancer?
使用一些不同的工具,医生诊断乳腺癌,通常开始像一个乳房X线照片成像测试。
Imaging
- 乳房X光摄影:大多数妇女应该开始得到规则screeningmammograms in their 40s, although high-risk women may need to start earlier. These x-ray imaging tests look for masses or small white dots known as calcifications. If a doctor suspects breast cancer, they will order adiagnostic乳房X线照片以进一步探讨在乳房的任何变化。在诊断乳房X光检查,放射科医生会经常看图像立即,你需要等待,如果他们要采取额外的照片,或者他们会在一个地区使用尤其是“放大”的观点,真正零。
- 超声:Sometimes the doctor will want to get a different or more-detailed picture of your breast and will order an ultrasound or magnetic resonance imaging (MRI) to get more information about a suspicious lump or spot. Ultrasound is a great option for following up on a suspicious lump because the sound waves bounce back differently off a fluid-filled cyst versus a solid lump that’s more likely to be cancer.
- 磁共振成像(MRI):妇女谁是患乳腺癌的高风险有时需要一个MRI与他们定期乳房X线照片一起。这是因为核磁共振成像可以“看到”一些癌症是乳房X光检查会错过。这就是说,跳绳乳房专用,只是有一个MRI是不是一个好主意,因为MRI能错过其他癌症,将出现在乳房X光检查!
活检
在一个切片检查,医生会采取一些流体或组织从乳房,并测试其异常。有几个不同类型的活检:
- 细针穿刺:在这种最小侵入性的选项,一个医生将一个瘦小的,空心针入肿块移除一些细胞。(如果肿块是很难感觉或发现,医生有时会使用超声成像帮她知道在哪里的目标。)
- 切除活检:Just like is sounds, this one is more like surgery. A doctor will cut out the suspicious lump entirely and test it—this is the most accurate way to diagnose, or rule out, cancer.
Pathology Tests
如果活检显示,肿瘤是癌,医生会运行其他测试,以弄清楚它是什么类型的乳腺癌。许多不同的肿瘤特征影响预后和治疗,包括:
- 激素状态:Breast cancers that depend on estrogen or progesterone to grow are called hormone receptor-positive tumors. These cancers can be treated with hormone-therapy drugs and often have a better prognosis than other tumors, according to the American Cancer Society. A majority of breast cancers are hormone-receptor positive.
- HER2状态:HER2阳性乳腺癌过量产生HER / neu蛋白,这可以加速肿瘤的生长。这些谁试验阳性接收某些有针对性的药物治疗,可以阻止这些信号。
如果这两个激素受体和HER2测试呈阴性反应,乳腺癌被列为三阴性。他们往往比其他类型的乳腺癌更积极,尽管专家们不知道是什么原因,也有较少的针对性的治疗。
什么是最好的治疗乳腺癌?
Most breast-cancer treatment includessurgical removal的肿瘤。但许多人需要更多的关心after that. The best combination of treatments for your breast cancer depends on the type and stage, and your own preferences. A lot of people consult with a team of different types of doctors including oncologists and breast surgeons before deciding what to do.
Surgery
- Lumpectomy:Just the tumor and some of the tissue around it is taken out. This can be a good option for people with cancers that are small, relative to the breast and are not multiple within the breast. Many patients with spread to nodes may also be candidates.
- 乳房切除术:所有的乳房组织(和乳房有时乳头和/或皮肤)被去除。它通常建议当有乳房癌几个方面,或者在比较健康的乳房组织量的肿瘤是非常大的。
- 淋巴结清除术:去除部分或全部腋下淋巴结。如果肿瘤已经扩散到乳房本身,这可能是必需的。
药物
- Chemotherapy medications用于杀死或收缩癌细胞。有些肿瘤反应比你的具体癌细胞做会帮助你和你的医生决定这些药物是否应为您的治疗计划的一部分,其他的测试以化疗。化疗通常被给定为静脉滴注or injection at a clinic or doctor’s office. Doses are given in bursts—or cycles—of a few weeks at a time so that patients are able to rest and recover from each treatment before having another. The length of time a person will need chemotherapy treatments can vary, but it often lasts anywhere from three to six months.
- 激素治疗are often used to treat hormone-positive cancers in order to cut off the supply of hormones the tumors need to grow and spread. These medications are usually taken for a long time—between five and 10 years.
- Other medications可以用来鼓励一个人自身的免疫系统来杀死癌细胞或靶向在一些癌症特异性蛋白质(如HER2阳性肿瘤)。而不是杀死癌细胞的方式,不化疗,靶向治疗通常不损害健康细胞一样多。靶向疗法可作为注射剂,输注IV,或药丸形式和一些可给予最多的一年。
Radiation
非常高能X射线,以消灭癌细胞,缩小肿瘤,和/或帮助预防乳腺癌从不断增长的手术后回到传递到乳房。无论您需要的辐射取决于很多因素。如果你有一个乳房肿瘤切除术代替乳房切除术的,例如,您可能需要辐射扎普可能已留下任何恶性细胞,降低肿瘤能重新长出来的机会。有些妇女需要辐射乳房切除术后,以及。
辐射是对你整个乳房要么完成了,或只是其中肿瘤所在的部分。如果你的医生决定,你需要全乳照射,你会得到一个治疗五天,每周三到六周。如果你的乳房只有部分需要辐射,您通常需要一天一次或两次治疗三到五天。
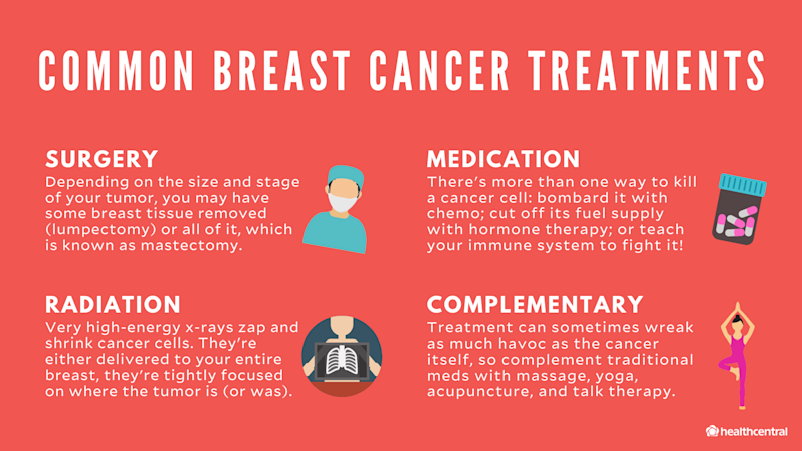
治疗可以帮助其他类型
有a reason people talk about the war against cancer: Because treatment turns your body into battleground. So when you’re going through it, do whatever you need to feel comforted, supported, and less stressed out. Massage, yoga, acupuncture, and/or plain old therapy can be the balm that protects you from any collateral damage.
乳腺癌的每个情况都不同,所以是每一个治疗计划。详细了解乳腺癌的治疗可能会适合你。
Read MoreDoes Breast Cancer Treatment Cause Complications?
它可以。不同的治疗方法有不同的风险和副作用,但这些都是一些最常见的,根据CDC:
Surgery
- 痛
- 胸部感觉丧失或剩余乳腺组织
- A type of swelling called lymphedema. After having radiation therapy—or lymph nodes removed during surgery—lymph fluid can start building up in the arms, hands, breasts, or torso.
Chemotherapy
- 恶心
- Mouth sores
- 脱发
- 感染的高风险
- Reduced appetite and/or weight loss
- Brain fog or trouble with concentration and memory (often called “chemo brain”)
激素治疗
- 头痛
- Mild nausea
- 潮热
- 阴道干涩
- 阴道分泌物
- 潮热
- Night sweats
- 增加血液凝块的风险
- Mood swings
Targeted Therapies
- 疲劳
- 脱发
- Mouth sores
- 恶心
- 增加胆固醇或血糖
- Increased risk of infection
- 心脏问题
乳腺癌治疗的副作用可能会非常不愉快,但这些天,医生有很多方法来帮助缓解,从抗恶心药物,以那些提高你的免疫力。不要担心把一个勇敢的前面。如果你有症状的挣扎,让你的医生知道,使他们能够帮助你找到一些救济。
什么是生活像人们患乳腺癌?
活一天到一天被诊断出患有乳腺癌后,可充满了恐惧和焦虑,再加上疼痛或治疗其它真的 - 不好玩的副作用。您可能还需要对付的人谁不明白的情况并不能完全掌握你正在经历什么。但这里有一个好消息:因为乳腺癌是一种比较常见的疾病,因为有这么多优秀的治疗方法,也有很多人谁了解你的情况,可以帮助的人。
Take things one step at a time: Educate yourself about breast cancer, never be afraid to ask your medical team questions, and enlist the help of a friend or loved one to go to appointments with you. Breast-cancer treatment can be complex and the terminology confusing. It can be hard to keep everything straight when you are feeling unwell or are scared—your appointment buddy can take detailed notes and write down questions for you to ask next time.

Emotional Health
这种诊断可以改变你的生活天翻地覆。但是你要进行一些你的生活在未来数个月,压力和抑郁的最重要的决定可以与你的愈合过程产生干扰。以下是如何进行反击。
- 工作应力释放到你的日常生活。负面情绪会影响你做出决定周到,以及导致的应力,可以抑制你的免疫系统的能力。所以一定要结合活动,帮助你平静你的心灵,如冥想,深呼吸,锻炼日记,或任何其他方法,对你的作品。
- 说出来!与你正在经历可以帮助你不那么寂寞的朋友和家人聊天。它也将让他们有机会提供支持。当他们这样做,把它。如果你是太累了,做饭,让他们带给你的晚餐。如果你想在公司化疗治疗,让他们的输液过程中开车送你到门诊和住院和聊天。
- Consider attending a support group or talking to a therapist. Being diagnosed with breast cancer is frightening—even if yours is caught early and you have a sunny prognosis. No one can understand exactly what you’re going through quite like someone who’s experienced it. Many larger hospitals and cancer centers have free support groups for patients. Try one out.
性生活
癌症involves you in the fight of your life, and it’s often difficult to think about anything else, including sex. Plus, the way you feel about your body and how it looks can change a lot after lumpectomy or mastectomy surgery. Treatments like chemotherapy or hormone therapy can also interfere with sexual desire or function. But you don’t have to just sit back and take it. A good first step is to talk to your doctor. Most women deal with some sex-life changes and interruptions during or after breast-cancer treatment. Your doctor will not be surprised or embarrassed when you bring it up! And she can help: There are medications and other fixes she can recommend to help ease sexual side effects of medications; plus she can refer you to a support group for other breast-cancer survivors or to a counselor who is skilled at helping survivors ease back into their normal lives—orgasms included.
在哪里可以找到乳腺癌的社区?
有a lot of talk about breast cancer but finding and talking to people who know究竟what you’re going through can be just as important as finding a treatment plan that works. Here are some places to start to make connections, find resources, and meet friends.
Top Breast Cancer Bloggers/Instagrammers
- 布兰妮比德尔,@brittneybeadle
Follow because:乳腺癌不排除她的生活,她继续鲜活的生命发挥到淋漓尽致,只有“一触摸的转移性乳腺癌“。有一天,她在化疗,第二天,她基本上是谁在海边住了一条美人鱼。
- 玛吉Kudirka,@baldballerina,baldballerina.org/
Follow because:她从大舞台去为与Joffrey的一致行动集团在纽约芭蕾舞演员,对化疗IV期转移性乳腺癌的椅子。随着她的身后双乳切除术,她的战斗力和扣她的途中回到聚光灯下,一个plieat a time.
- Dayna DONO,@daynadono,anaono.com/
Follow because:有actually一个胸罩和她是一个要感谢它。她是AnaOno,胸罩的创办人兼设计师专门针对谁曾乳腺癌的妇女重建,乳房整形,乳房切除术制成,或生活在,只是不与其他胸罩以及混合其他条件。
- Umi Marie,@umi_kmarie
Follow because:炫舞,瑜珈,三妈,和乳腺癌的战士 - 这些都只是一些她的头衔。但是,当我们滚动她的饲料,我们看到:诗人。她感激的话,鼓励像小咒语被你的生活 - 和他们中的很多从她的存活干。
- 贝丝仙童,@bethfairchild
Follow because:她的无畏和战斗Ⅳ期乳腺癌。她的广告活动,乳腺癌的认识是新鲜的,不胫而走,而且我们完全鼓励你开辟这条道路与她。
- Nalie Agustin,@nalieagustin
Follow because:YouTube用户动机奥古斯丁Nalie在刚刚24岁确诊为IV期乳腺癌。她vlogged一路走过她的治疗自己的频道,然后开始The Nalie Show在那里,她会谈同胞癌症幸存者,名人和其他鼓舞人心的乡亲。
- 萨布丽娜老八,@sabrinaskiles
Follow because:We might be biased since she’s aHealthCentral columnist, but we’re thinking — no, we知道— you’re going to adore her just as much as we do. Not that long ago she was a 30-something mom of two boys, following her husband across the country for his dream job, and celebrating a milestone birthday. That all changed overnight when she found a lump in her breast. Now she’s a beautifully mixed bag of mom-chemo-wig-wife-radiation-recovery-life. Her posts, like mini columns, will leave your heart either broken, fulfilled, or both, all at once. Oh, and she shares breast-cancer-friendly recipes, too! Told you she’s worth the follow.
- Bree Jordan,@cancerwontstopbree
Follow because:她的Insta生物说明了一切:她是“一个艰难的母亲,战斗乳腺癌和抚养一个孩子。”Without even reading her words (which will also suck you in), the pictures you’ll find while scrolling her feed are so powerful and will draw you in (like the one of her with a full head of hair looking over at herself, now bald #chills). You see the tough parts of chemo, but also how she fights to bounce back in life — like hopping on her cycle bike the day after her first chemo treatment.
- Jessica Boyd,@jessicaaboyd
Follow because:仅仅因为她是几年后从她最后一轮化疗的,并不意味着她停止战斗中最难打她的生命对抗癌症复发。尤其是当她有一个理由来打 - 为她的奇迹宝贝,完成癌症治疗后怀孕三年。加入她在每月的第一天为一个自我乳房检查(不要担心,她会提醒你),并在她的健身旅程强留,让她可以抵御转移性乳腺癌。
前乳腺癌播客
- The Cancer Game Plan。该周报显示谈话到一个新的鼓舞人心的癌症战士每周对他们的旅程加上他们的“搞笑”瞬间癌症和癌症患者生活顶级技巧的主机。
- Investigating Breast Cancer。本届车展,从乳腺癌研究基金会,讨论了在该领域顶尖医生最新的乳腺癌的消息。
- 精简和直了尼克Austman。Two-time breast cancer survivor and certified life coach helps you juggle a Jekyll-and-Hyde life of depression and laughter—because the balance is real when you’re living with breast cancer.
- 癌症,随便。最充分的总编辑和乳腺癌幸存者林赛·德隆带来了一些显着的和勇敢的客人帮助thrivers继续通过其他的肠道痛苦或鼓舞人心的旅程一枝独秀。以新的视角走开的“大C.”
- 在良好的辉光。她的乳腺癌诊断后,乔治·克劳福德的生活观点完全改变了。她需要一个新的面貌,一个把她带回了自我保健的基本知识,并积极与自己周围。这听会给你所有的好共鸣。
- 巨蟹座的营养师播客。没有说癌症治疗像良好的营养,他们基本上在治疗过程中它推了你的喉咙(几乎字面意思)。朱莉兰福德,R.D.,告诉你,正是你需要给你的身体,无论你是在治疗的时候,一个幸存者试图避免复发,或者你有乳腺癌的家族病史,并试图保持领先的赔率。
前乳腺癌支持团体和非营利组织
- Living Beyond Breast Cancer。可靠的信息,社区,并为患有乳腺癌和他们的朋友和家人,加上如会议和研讨会现行教育方案的支持。还有一个免费的在线/电话服务热线,将符合患者的志愿者一对一的支持和教育。
- 年轻的生存联盟。该YSC特别关注人40岁以下,免费教育计划和指南加上活跃的讨论区,一个私人facebook群体,而在人的聚会受到乳腺癌。
- Susan G. Komen Breast Cancer Foundation。其中最知名的乳腺癌倡导组织,科曼是乳腺癌研究重地募捐,并从在线处理导航工具的乳房护理服务热线和有关财政援助中提供广泛的免费服务。
- Metastatic Breast Cancer Network。以病人为主导的宣传组织,专注于独特的需求和生活转移性(或IV期)乳腺癌的人的关注。该MBCN提供的临床试验和治疗晚期乳腺癌,同伴支持小组和留言板,甚至资金的科研信息。
- 该Breasties。它们使乳腺癌看起来酷。“自由撤退s, events, and community for women affected by breast and reproductive cancers.”
- 愚蠢的哑乳腺癌在Facebook上。A community of women going throuhg breast cancer at all different stages. You will get an answer and support on anything you post. Sweet, genuine women wanting to pay it forward and support others.
经常问的问题乳腺癌
How do I check myself for breast cancer?
The best way is to get to know your breasts—how they feel, what they look like, and how they change during your menstrual cycle—and to let your doctor know about any concerning changes. The most common symptom of breast cancer is a lump. Other signs can include dimpled skin, pain or swelling in one breast that's not related to your period, skin inflammation, and unexpected nipple discharge.
What are the chances that I could develop breast cancer?
每个人的风险是不同的,取决于多种因素,如遗传,家族史,生活方式等问题。但女性平均拥有约在她的生活中患乳腺癌的12%的机会。诊断的年龄中位数为62;只有约5名妇女患乳腺癌%被确诊40岁以下。
什么是乳腺癌生存率?
预后取决于多种因素,包括肿瘤的分期,肿瘤的类型和治疗提供什么。但平均而言,浸润性乳腺癌的五年存活率为90%。10年生存率为83%。转移性乳腺癌(已经扩散至身体的其他部位的类型)的5年存活率为27%。但要记住,乳腺癌的早期形式的成活率为99%。
男人得乳腺癌?
Yes. Any person of任何性别可以得乳腺癌, although women are 70 to 100 times more likely to develop the disease than men, according to the American Cancer Society. About 2,600 men are diagnosed each year.
- 乳腺癌发病率:美国癌症协会。(2019)。“癌症事实与数字2019”cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf
- Stages of breast cancer:美国癌症协会。(2019)。“American Cancer Society Guidelines for the Early Detection of Cancer.”cancer.gov/about-cancer/diagnosis-staging/staging
- 的DCIS案件进展为癌症的估计:临床肿瘤学杂志(2018)。“手术比较,以监测和内分泌治疗的低风险DCIS(COMET研究)。”ascopubs.org/doi/abs/10.1200/JCO.2018.36.15_suppl.TPS599
- 第IV阶段癌症慢性疾病:美国癌症协会。(2019)。“管理癌症慢性疾病。”cancer.org/treatment/survivorship-during-and-after-treatment/when-cancer-doesnt-go-away.html
- Who should be tested for BRCA mutations:UpToDate. (2019). “Recommendations from the United States Preventive Services Task Force on who should be offered genetic testing for BRCA mutations.”uptodate.com/contents/image?imageKey=ONC%2F57434
- 风险因素:疾病预防与控制中心。(2019)。“乳腺癌:有哪些风险因素?”cdc.gov/cancer/breast/basic_info/risk_factors.htm
- 在第一期和风险年龄:苏珊科曼。(2019)。“年龄在第一次的时期。”komen.org/BreastCancer/FirstPeriodOccursBeforeAge12.html
- Oral contraceptives and risk:美国国家癌症研究所。(2019)。“Oral Contraceptives and Cancer Risk.”cancer.gov/about-cancer/causes-prevention/risk/hormones/oral-contraceptives-fact-sheet
- Body fat and risk:JAMA Oncology。(2018). “Body Fat and Risk of Breast Cancer in Postmenopausal Women with Normal Body Mass Index; A Secondary Analysis of the Women’s Health Initiative Randomized Clinical Trials and Observational Study.”ncbi.nlm.nih.gov/pmc/articles/PMC6439554/
- When to get a mammogram:美国癌症协会。(2019)。“American Cancer Society Guidelines for the Early Detection of Cancer.”cancer.org/healthy/find-cancer-early/cancer-screening-guidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer.html
- 乳腺癌的症状:美国癌症协会。(2019)。“乳腺癌的症状和体征。”cancer.org/cancer/breast-cancer/about/breast-cancer-signs-and-symptoms.html
- 乳腺癌的治疗:美国国家癌症研究所。(2019)。“乳腺癌治疗(成人)(PDQ)-Patient版本。”cancer.gov/types/breast/patient/adult/breast-treatment-pdq#_222
- 治疗的副作用:疾病预防与控制中心。(2019)。“癌症治疗的副作用。”cdc.gov/cancer/survivors/patients/side-effects-of-treatment.htm





